The new Last Orders episode is out, featuring me, Tom Slater and Roby Lyons. This month it's a special 'Everything's Coming Up Snowdon' edition in which we only discuss good news: Public Health England, Turkey Twizzlers, the end of prohibition in South Africa and the success of Sweden.
Friday 28 August 2020
Friday 21 August 2020
Meaningless graphics
Last year I started curating a Twitter thread of meaningless, stupid and pointless graphics, mostly Powerpoint slides from 'public health' conferences. The thread has become difficult to follow so I'm putting them all here and will add to them from time to time.
Thanks to everyone who has submitted entries. Keep them coming.
1. The umbrella of health (from the EAT-Lancet commission)
2. The Doughnut (plus added random statistics at the bottom). I am told that this graphic is highly revered in some circles.
3. The Bicycle of Education
4. With great power comes 97% responsibility.
5. The Non-Communicable Disease Policy Cube
6. The Bicycle of Disease Prevention
7. Another one from EAT-Lancet. You could stare at this from now until the end of time and be none the wiser.
8. A simple guide to COVID-19 from Danny Dorling
9. The Sisyphus of Something
10. Food, brain, stomach.
11. God knows.
12. Evidences based research, medias and economical interest. This is from the World Health Organisation.
13. Obesity simplified.
14. Perhaps you had to be there.
15. Should have been bullet points.
16. Everything but the kitchen sink.
17. Something to do with industry being connected to policy makers.
18. Muh capitalism.
19. Muh corporations.
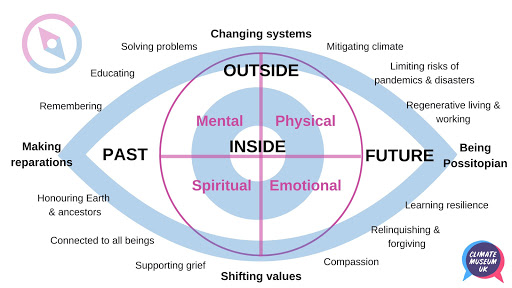
20. The Eye of Possitopianism.
21. The teepee of innovation.
22. Formula for peaceful societies revealed.
23. Feeling sleepy.
24. "Any questions?"
25. The 'whole systems approach' to obesity. Absolute drivel.
26. People and actions.
27. The World Economic Forum, bullshitters extraordinaire.28. How to prevent littering.
29. 'System change leaders' 🤮
30. Some more gibberish from the NHS.
31. How to solve a problem.
31. We are all one.
32. A banger from the renowned political thinker Paul Mason.
33. They love circles, don't they?
34. The doughnut but in French.
35. Asses.
36. From Viz.
37. Nailed it.
Wednesday 19 August 2020
RIP Public Health England. Where next for 'public health'?
You may probably heard the news that Public Health England is to be closed down. As you can imagine, I nearly died laughing. It is a rare example of the government acting on a recommendation from an IEA report before the report has been published (coming in September).
But what now? What comes next?
I offer a roadmap in this article for the Spectator.
In his farewell email to staff, PHE’s chief exec Duncan Selbie wrote that the ‘obvious next priority is to secure the right and best future for all those other responsibilities of PHE that are not about health protection’. PHE’s empire building created many well remunerated jobs. Those who are on the low-fat gravy train will be understandably reluctant to get off and will be lobbying hard for a new agency that is Public Health England in all but name. Having set up the National Institute for Health Protection, the government may be tempted to set up a twin organisation, perhaps called the National Institute for Health Improvement (although Nanny State England has more of a ring to it).Politicians love creating new bureaucracies, but they should resist the urge.
Sunday 16 August 2020
Political pygmies
The Scottish government is banning music in pubs on the flimsy grounds that people might raise their voice and spread the coronavirus. It is the latest in a series of petty measures from pygmy politicians. I discuss some other articles in this article for the Telegraph.
None of these policies, not the ban on smoking outdoors, nor the ban on the sale of e-cigarettes, nor the restrictions on food sales, will have the slightest impact on Covid-19 (except, perhaps, negatively). The only thing they have in common is that political pygmies have always quite liked the sound of them.
Faced with a serious public health problem, unserious people have retreated to their comfort zone of trivial lifestyle regulation. They cannot change the record. They were not made for these times.
I also discuss a recent study that claimed vaping greatly increases the risk of contracting the virus.
Written by three Californian academics, one of whom is the founder and director of an anti-vaping organisation, the study produced the unlikely finding that e-cigarette users are five times more likely to test positive for Covid-19. There is, to put it mildly, no obvious biological mechanism for this and the explanations offered by the researchers were risible.
They suggested that vapers were at greater risk of contracting Covid-19 because they touch their mouth and face more (they don’t), or because vaping causes the same damage to lungs as smoking (it doesn’t), or because vapers share devices with one another (even the authors admit that this was unlikely to happen much under lockdown).
The study’s methodology left a lot to be desired. It was based entirely on an anonymous online survey of 13 to 24 year olds. None of the information could be verified and we do not know how the respondents were recruited. The number of self-reported vapers who self-reported a positive Covid-19 test was so small (50) that it would have been easy for anti-vaping activists to game the system with fake responses.
Moreover, the association between vaping and Covid-19 only existed for people who had used an e-cigarette in the past. Inexplicably, there was no such association for people who had used an e-cigarette in the past 30 days (nor, indeed, for people who smoked).
Saturday 8 August 2020
Smoking and COVID-19 - the evidence gets stronger
I've found it impossible to keep up with all the research on smoking and COVID-19 recently. The tireless @phil_w888 has now catalogued over 700 studies of COVID-19 patients that have data on smoking prevalence.
In the last week, the largest observational study yet conducted found that smokers (in Mexico) were 23 per cent less likely to test positive for COVID-19. This is in line with the results of an ongoing meta-analysis by some researchers who would clearly prefer the hypothesis to be disproved but who nevertheless have found a 26 per cent reduction in infection risk for current smokers.
A study published in the Lancet a couple of weeks ago looked at the factors associated with COVID-19 caseloads at the national level. It found that countries with higher rates of smoking tended to have lower rates of Covid infection.
And a newly published prospective study of nearly 20,000 Covid cases tells a familiar story. Your chances of ending up in intensive care with the virus are increased if you are male, non-white, from a low income area, obese ... or a nonsmoker.
Note the telltale dose-response relationship. The heaviest smokers are an incredible 88 per cent less likely to end up in ICU with COVID-19.
The same rules apply to your chances of testing positive for COVID-19. Indeed, it seems increasingly clear that smokers are less likely to end up in intensive care with COVID-19 because they are less likely to catch it in the first place.
Factors such as obesity, deprivation and being BAME are now universally acknowledged as risks for COVID-19. The UK government, in particular, has gone to town on the obesity finding.
The smoking finding, by contrast, continues to be ignored, although the evidence for a protective effect is about as a strong as the evidence for obesity being a risk factor.
And yet the association with smoking is not even mentioned in the abstract of the latest study (above), nor is it mentioned in the abstract of the Lancet study. The authors of the latter describe it as an 'unexpected finding' which 'requires further investigation'. The authors of the other study describe it as a 'counterintuitive finding' , although they do acknowledge that it is 'consistent with very low rates of smoking seen in patients presenting with COVID-19 in Wuhan and similar data from the USA and with the findings of a more limited analysis of patients with COVID-19 in France.
They also propose several possible causal mechanisms:
This may reflect a general immunomodulatory effect, a mechanism that is thought to explain the lower incidence of sarcoidosis, extrinsic allergic alveolitis and ulcerative colitis in current smokers. Alternatively, smoking may cause increased ACE2 mRNA expression in human lung much as ACE inhibitors or ARBs are believed to, suggesting a possible common protective mechanism for severe COVID-19 disease. Additional possible mechanisms include a direct protective effect of nicotinic receptor stimulation or an association of smoking with another protective factor. This finding arose when including smoking status as a confounder and should be interpreted cautiously. Further studies are required to verify the apparent protective association, determine whether it is independent of other risk factors, and investigate potential mechanisms.
The 'public health' lobby has done a good job of ignoring these findings so far, but how long can it continue? With the world economy crippled by lockdowns and social distancing - not to mention the human cost of the virus - is it ethical for them to overlook a possible solution? That solution may not involve smoking per se. It is likely to merely involve harmless nicotine.
These findings get stronger by the day and are extremely interesting, and yet I do not see much interest in them from the people who are supposed to be protecting our health. It could be a fatal oversight.
UPDATE
Imperial College's antibody testing study arrived at a familiar finding:
Those who were overweight or obese had higher prevalence than those with normal weight, and current smokers had a lower prevalence than non-smokers (3.2% vs. 5.2%(OR 0.64 [0.58,0.71])
That's a 36% lower risk.
Monday 3 August 2020
Remain (Inside) vs. Leave (the House) - the faultline in British politics
On the face of it, the two issues have nothing in common. It may be that Brexiteers are less risk averse. No Deal Brexiteers, in particular, embrace risk almost by definition. Remainers, by contrast, feel safer with the status quo, and once lockdown became the status quo, any loosening of it felt like a risk.Or it could be about settling old scores. Some pro-lockdown campaigners are more or less explicitly anti-Tory activists who oppose any relaxation so they can say ‘I told you so’ in the future when there is a second wave of (hello, ‘Independent SAGE’).
Others are still smarting from the referendum. I swear there are political journalists in this country who will go to their graves convinced that the biggest news story of 2020 was Dominic Cummings driving to Barnard Castle. It is difficult to imagine them getting quite so upset about a special adviser possibly committing a minor breach of a regulation if he had not run the Leave campaign.
Similarly, it is hard to imagine Sir Ed Davey reporting someone to the police for going to the pub two weeks after travelling to America - and therefore possibly not having quite done the full fourteen day quarantine - if his name wasn’t Nigel Farage (or as Carole Cadwalladr dubbed him, in typically understated fashion, ‘Typhoid Nigel’). Farage’s response was to tell Davey, not unreasonably, to ‘get a life.’
Do read it all.
Saturday 1 August 2020
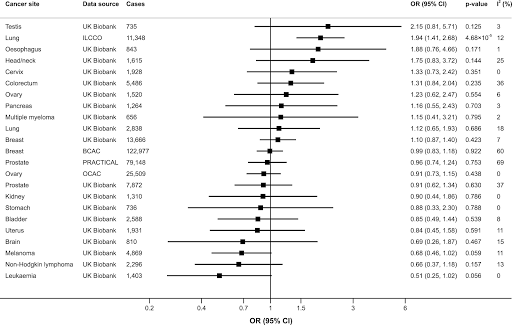
Alcohol doesn't cause cancer?
And then last week, an MR study published in PLOS Medicine failed to find an association between inferred alcohol consumption and any form of cancer except - using one of the two databases - lung cancer.