There was much excitement in 'public health' circles last year when a study failed to find an association between moderate drinking and lower rates of heart disease. The study used conventional epidemiology and Mendelian Randomisation (MR) to look at a Chinese population in which a gene that is associated with alcohol avoidance is relatively common (it is very uncommon in the West). The authors found a protective effect for heart disease when they used epidemiology but not when they used MR. It was not the first MR study to come to this conclusion.
MR studies featured prominently in the Sheffield Alcohol Research Group's report for the Australian government last year (Australia has since lowered its drinking guidelines). They also feature prominently in the US Dietary Guideline Advisory Committee's report (the US is also pondering a lowering of the guidelines). You can see the appeal to the anti-alcohol lobby.
The hype around MR studies says that they are 'nature's RCTs' and can prove causation. Neither of these claims is true, at least as far as identifying behavioural risk factors is concerned. Observational epidemiology is far from perfect but MR studies have enormous problems of their own. Self-reported alcohol consumption data might not always entirely reliable, but MR often does not involve alcohol consumption being reported at all. It is merely assumed that people with certain genes will drink less than other people.
But just as someone whose genes make them more likely to smoke is not necessarily a smoker, someone who has genes that make them more prone to alcohol avoidance is not necessarily a non-drinker (or even a light drinker). A few genes have been identified, particularly in Asian populations, which make people react badly with alcohol, but this is no guarantee that they will not drink heavily. In situations and cultures in which drinking is expected - networking among Japanese businessmen, for example - any genetic predisposition towards light drinking or teetotallism may soon evaporate.
In a
commentary in the European Journal of Epidemiology, Kenneth Mukamal and
colleagues argue that MR “is subject to all of the limitations of
instrumental variable analysis and to several limitations specific to
its genetic underpinnings, including confounding, weak instrument bias,
pleiotropy, adaptation, and failure of replication.” MR studies on
alcohol consumption and cardiovascular disease, they write, “demonstrate
that it must be treated with all of the circumspection that should
accompany all forms of observational epidemiology”.
Two new MR studies were published recently, neither of which attracted much attention. In June, an MR study published in Cancer Genetics found no association between inferred alcohol consumption and breast cancer. It also found no association with ovarian cancer.
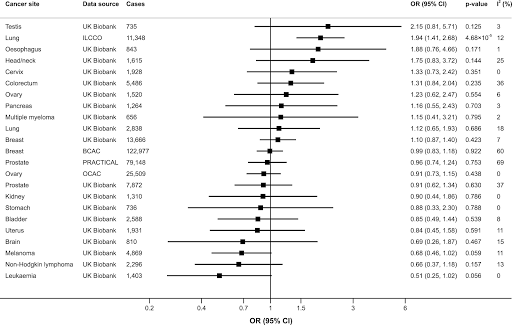
And then last week, an MR study published in PLOS Medicine failed to find an association between inferred alcohol consumption and any form of cancer except - using one of the two databases - lung cancer.
And then last week, an MR study published in PLOS Medicine failed to find an association between inferred alcohol consumption and any form of cancer except - using one of the two databases - lung cancer.
The PLOS study is particularly interesting because it also looks at smokers - or, more accurately, people with a genetic predisposition to smoking. If it hadn't found an association with lung cancer, it would have raised serious questions about MR's credibility in this area. Fortunately it did, but it only found a doubling in risk, whereas epidemiological studies suggest that risk increases by anything from five to fifty-fold depending on smoking intensity. The study also found associations with several other cancers, but the risk ratios were quite low. For most of the cancers studies, there was no statistically significant association.
The results for inferred smoking therefore point broadly in the right direction, but it seems that the risk has to be rather large for MR to show a statistically significant result.
The results for alcohol, however, would require the textbooks to be rewritten if they were true. The epidemiological evidence linking alcohol to several forms of cancer
is nearly as strong as the evidence linking moderate drinking to lower
rates of heart disease. Lung cancer isn't one of them, but that is the only cancer with which the MR study found a statistically significant elevation in risk, albeit in only one or the two datasets used.
What are we to conclude? That MR has 'proven' that moderate drinking does not reduce heart disease risk, but that drinking in general does not increase cancer risk? Or that MR studies are too crude to find the kind of associations identified by observational epidemiology - including the link with breast cancer which is the basis of the 'no safe level' meme?
If we are to allow MR studies to override
epidemiological findings about alcohol, several babies will have to be thrown out with
the bathwater.


No comments:
Post a Comment
Comments are only moderated after 14 days.