If heavy exposure to Risk Factor X increases risk of Disease Y by 200%, and moderate exposure increases risk by 10%, a layman might decide to focus on those who are mostly heavily exposed because they are at greatest risk.
Not so fast, says the 'public health' expert. Only 1% of the population are heavily exposed whereas 60% of the population are moderately exposed (the other 39% avoiding exposure altogether). This means that moderate exposure accounts for more cases than does heavy exposure. Efforts should be focused on those who are moderately exposed.
This makes a certain amount of sense in the theoretical example above, but it is not a principle that can be universally applied. Rose tried to apply it to all sorts of risk factors and his successors have applied it to more, including gambling and salt consumption.
Doctors tend to deal with people on the extremes: alcoholics, the morbidly obese, people with very high blood pressure, etc. Rose's version of preventive health focused on the (median) average person. There are a lot of people at or around the average and not so many at the extremes. His view that you save more lives if you focus on the apparently 'normal' than on the high-risk 'deviants' gave licence to the 'whole population approach' of government imposing broad-brush policies on everybody.
Leaving aside the negative consequences of these policies, the theory only works when the average person is at genuine risk. Take blood pressure, for example. The first graph in Rose's book shows the bell curve of systolic blood pressure. The y-axis is the percentage of population.
From this we can see that the median adult has a reading of around 130/80mmHg. On the right-hand tail of the distribution we can see the people who have high blood pressure.
In Rose's view, you would save more lives by lowering the blood pressure of people who had a reading of 120 or 130mmHg than by treating the people whose blood pressure exceeded 160mmHg. Why? Because there are so many more of them.
He complained that doctors only considered giving statins to people whose blood pressure exceeded 100mmHg - thus 'encouraging the belief that those who do not qualify for the high-risk group, because they are "normal", have no cause for concern.' (p. 47).
But is there cause for concern? What reason was there to think that the blood pressure of an average person was unhealthy? One of Rose's own graphs shows that the risk of heart disease does not increase until blood pressure exceeds 130mmHg.
Weirdly, Rose claims that this graph shows 'a continuum of associated risk which increases progressively over the whole observed range'. It does not. It shows that the baseline rise is about 6% and that risk only begins to increase from around 130mmHg.
Of course, there are occasions when being 'normal' or average is not healthy or, at least, not optimally healthy. Rose gives the example of average cholesterol levels in Finland, which are (or were) a lot higher than levels in Japan. The former is probably less healthy than the latter.
But it cannot be assumed that the average person everywhere is always at elevated risk, nor that their health would invariably benefit from doing less of whatever it is that carries risk to people on the extremes.
Take alcohol. The physical harms of alcohol overwhelmingly affect (a) people who get very drunk and suffer acute harms, and (b) people who drink a great deal for many years and suffer chronic harms.
The average drinker does neither. Even if we leave aside the J-Curve showing significant health benefits from moderate consumption, it is clear that alcohol consumption by the median drinker contributes only a very small part to alcohol-related ill health.
This is a challenge to Rose's theory and therefore to the whole population approach. This is awkward because it is in the field of alcohol that the whole population approach has been most warmly embraced. It is officially endorsed by the Scottish government and is at the heart of Ireland's Public Health (Alcohol) Act which will restrict advertising, introduce minimum pricing, put alcohol behind shutters, etc.
How can this be justified? Step forward Claire O'Dwyer and her colleagues from Ireland's Health Research Board. Last week they published a paper title 'Drinking patterns and the distribution of alcohol-related harms in Ireland: evidence for the prevention paradox' which includes a passage that is hilariously and shamelessly political, even by the standards of 'public health' activist-academia:
Policy implications
Research indicates that the most effective approaches to reducing alcohol consumption are those which target the entire population, such as increasing the price and reducing the availability of alcohol. In Ireland, the Public Health (Alcohol) Act (2018) has recently (October, 2018) been passed and will introduce a number of population-based strategies to reduce alcohol consumption, including a minimum unit price for alcohol sales and restrictions on advertising and marketing. This policy represents one of the most progressive alcohol policies in the world. It was fiercely contested by the alcohol industry and the interval between the publication of the Bill and the passage of the Act at 3 years was the longest ever in Ireland. None of the provisions in the Act have yet been implemented. The findings in this study demonstrate that alcohol-related harms in Ireland are distributed across the population, providing support for a population-based strategy to reducing alcohol consumption. The findings thus indicate a need for the rapid implementation of measures outlined in the Public Health (Alcohol) Act (2018).
Subtle, eh?
The study itself purports to show that most alcohol-related harms 'are accounted for by low- and moderate-risk drinkers' and not, as some might expect, heavy and dependent drinkers.
The authors surveyed 4,338 drinkers and asked them if they had suffered any harm in the last twelve months.
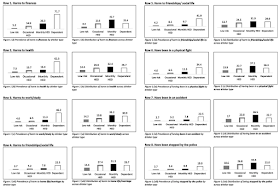
The eight harms covered were harm to finances, harm to health, harm to work or study, harm to friendships or social life, harm to home life or marriage, been in a physical fight, been in an accident, and stopped by the police. E.g., “Have you experienced harms to your finances in the last 12 months due to your own drinking?”
You will notice that only three of the eight relate to physical harm, including two (physical fights and accidents) which may not have necessarily resulted in any significant harm to health.
Indeed, even 'harm to health' does not necessarily imply significant harm to health. The journal that published the study, BMC Public Healthy, has open peer review so we can see that one reviewer asked the obvious question:
Question: how is 'harm to health' determined by the survey take? Does this refer to blacking out, or falling, or experiencing a hangover, or does this refer to receiving a clinical diagnosis, such as fatty liver disease?
The answer came back:
"Harm to health" was not further defined in the survey and was left up to participants’ interpretation.
So it could be anything from having a champagne cork fly in your face to being put in a wheelchair for life. It seems likely that most of these harms were relatively trivial because most accidents and illnesses are relatively trivial, but we have no way of knowing.
This runs the risk of producing apples and oranges comparisons. A dependent drinker developing acute pancreatitis counts for the same as a light drinker tripping over in a pub.
The results are below. Click to enlarge.
As the first and third columns show, dependent drinkers are much more likely to suffer 'harm' than the other drinkers. But only 6.9% of those surveyed were classified as dependent drinkers, so only a minority of the harmful incidents could be attributed to them (see the second and fourth columns).
The majority of incidents were accounted for by the other groups.
...these findings imply that most alcohol-related-harms are due to periods of acute intoxication, and because these occasions are most numerous among low and moderate drinkers, they account for the majority of alcohol-related harms.
There is sleight of hand at work here. The study does not look at moderate drinkers. It looks at moderate risk drinkers.
What is a moderate risk drinker? In this study, it is a non-dependent drinker who engages in Heavy Episodic Drinking (HED). Heavy drinking is immoderate by definition, I would have thought, and is defined here as the consumption of at least 60 grams of alcohol in one session (7.5 UK units, or about four pints of beer). The individuals could, of course, be drinking much more than that.
Moreover, they could be drinking much more than that very often. The survey asks how often the participant engages in HED. Regardless of whether they say “everyday”, “5–6 times a week”, “4 times a week”, “3 times a week”, “twice a week”, “once a week”, “2–3 times a month” or “once a month”, they are lumped together (see the black bar in the charts above) and considered to be 'moderate-risk'.
Common sense tells you that somebody who gets drunk most days is at high risk of all the 'harms' mentioned in this study, not least because the 'harms' in question relate to the consequences of drunkenness rather than the long-term effects on health. Somebody who only gets drunk once a month is clearly at lower risk and might be considered a low- to moderate-risk drinker by a layman (although not necessarily by a 'public health' academic). In this study, they are all grouped together as Heavy Episodic Drinkers.
It seems almost inconceivable that the survey didn't ask people how many units of alcohol they consumed, but if the authors have this information they don't use it. Why not? Units per week is the measure of choice in 'public health' for classifying risk. Many of the heavy episodic drinkers will be drinking enough for them to be classified as hazardous drinkers (more than 14 units a week) or harmful drinkers (more than 35 units a week for a woman or 50 for a man). It would be very useful to have this information.
The most cynical explanation for the authors' reluctance to show us how much these people are drinking is probably the correct one. If the statistics were broken down into subgroups, we would likely see a close association between heavy consumption and harm. Instead, the authors devised a methodology which allows people to consume vast quantities of alcohol and still be classified as 'moderate-risk' so long as they don't meet the DSM-IV criteria for alcohol dependence.
The study has another peculiar feature. For each of the harms, respondents...
...were assigned a score of 0 (“never”) 1 (“yes, once”) or 2 (“yes, more than once”) on each of the eight questions depending on their response. Scores on each of the eight harm questions were summed to give each participant a total score of harms that ranged from 0 to 16.
It is not clear how these scores were used in the final analysis, if at all. The results section only shows how many people had suffered each 'harm' at least once in the last year. This means that incidence of harm by, say, a dependent drinker who is habitually arrested and hospitalised will be greatly underestimated.
The authors are aware of this issue, saying...
This score is likely to be an under-estimation of harms, as “more than once” could equate to a number greater than 2.
But they justify it, saying...
However, the purpose of obtaining the total harm experienced by the survey population was not to provide a precise estimate of the number of alcohol-related harms in the population but was to estimate how the harms were distributed across each drinker type. Hence the scoring of the scale in this way was appropriate to the aim of the study.
Focusing on prevalence, rather than quantity, would be OK if the authors stuck to talking about prevalence. But they don't. On the contrary, they repeatedly insist that their findings show the proportion of incidents that are caused by each group. The abstract of the study says...
The majority of the harms in the population were accounted for by drinkers who were not dependent on alcohol... the majority of alcohol consumption and related harms in the Irish population are accounted for by low- and moderate-risk drinkers
This is wrong. The authors cannot make any claims about the number of harms. They can only make claims about the number of people involved.
This misrepresentation occurs again and again...
In line with previous findings on the prevention paradox, the majority of harms occurred to low-risk or moderate-risk drinkers...
...the majority of the harms were accounted for by people who engaged in HED...
...our findings indicate that the majority of harms in the Irish population were not accounted for by dependent drinkers...
The majority of alcohol-related harms in Ireland occurred among drinkers who engage in heavy episodic drinking.
When the study was picked up by the media, journalists naturally made the same mistake...
Binge drinking among low to moderate risk drinkers is responsible for most of the alcohol-related harm that occurs in Ireland.
None of these claims is supported by the study's results. The authors simply do not have the data to make such assertions. Under their methodology, a drinker who got into a fight at the Christmas party is responsible for the same amount of harm as an alcoholic who gets into fight every night.
This is a critical flaw because we know that a tiny minority of drinkers are responsible for a huge number of incidents. It should have been picked up in peer review, but neither of the reviewers even mentioned it.
In conclusion, let us return to the central claim of the study which I have already quoted above...
...these findings imply that most alcohol-related-harms are due to periods of acute intoxication, and because these occasions are most numerous among low and moderate drinkers, they account for the majority of alcohol-related harms.
It should now be clear that this is untrue for three reasons.
Firstly, the study barely examines the long-term health harms which are the cause of most alcohol-related mortality. At best, it shows that people who get drunk are more likely to be involved in situations that are associated with drunkenness than people who do not get drunk.
Secondly, the study does not look at 'low and moderate drinkers'. It looks at a poorly defined cohort of low and moderate risk drinkers, many of whom are neither moderate drinkers nor at moderate risk.
Thirdly, the authors can make no claims about 'most' or 'the majority' of alcohol-related harms because their study makes no attempt to quantify them.
So what does this study tell us about the prevention paradox? Nothing, because the prevention paradox is about death and disease, neither of which are measured here. Are moderate drinkers responsible for the majority of a broader range of harms? The data in this study is insufficient to tell us that either, but probably not.



No comments:
Post a Comment
Comments are only moderated after 14 days.